The advent of geriatric status in life is often accompanied by subtle changes in the mouth, which gradually increase to impact fundamental elements of healthy living.
Physiological Ageing involves:
. Decrease in total body mass, protein and water, bone density /osteoporosis.
. Sensory-motor deficit (reduced visual and auditory function).
. Decrease in liver, kidney and gastrointestinal function, taste and smell, heart and lung fitness.
. Decrease ability to metabolize drugs.
. Neuromuscular decline: reaction time, balance, strength of muscle tendons, ligaments.
Unfortunately, there is also an increased susceptibility to chronic systemicdisease, such as arthritis, cancer, COPD, diabetes, heart disease, hypertension, mental health conditions, osteoporosis, Parkinson’s disease, and Stroke, all of which have oral manifestations.
What are the common determinants ofpoor ORAL HEALTH in older adults?
Tooth mobility encourages pocket formation between the tooth surface and gum tissues.
This causes food accumulation and subsequent colonization by bacteria causing localized infection
Gingivitis/Periodontitiswith the potential for wider systemic infections.
advanced Periodontal disease, Gum recession
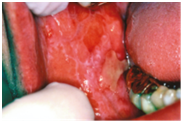
Friability of oral mucosa causes extreme sensitivity, easy bruising, either from minimal trauma (e.g., from sharp edges of denture margins) or nutritional deficiencies.
Missing teeth, dry mouth, and ill-fitting dentures makes eating, communication and social interaction challenging in the elderly.
Extreme tooth erosion, attrition defectsfrom wear-out process and faulty bite patterns over time
Root cariesis the involvement of less resistant root surfaces by extensive decay defects, increasing risk if rapid pulp involvement.
Decreased motor ability affects tongue function causing difficulties in speech, swallowing, traumatic cheek/lip bite, nocturnal mouth breathing that can lead to a form of sleep apnea. Difficulty in swallowing may lead to entry of food in the windpipe, and risk of fatal choking.
Oral Mucosal Lesions general immune response and healing capability of geriatric patients are poorer.
Painful Ulcers of Lichen Planus.
Increased incidence of Neoplasms, often metastasis from other body organs are visible in the mouth
Burning mouth syndrome
Oral candidiasis is commonly encountered among denture wearers, in debilitation, diabetes, anaemia, in those receiving chemotherapy or local irradiation, in patients on corticosteroids, broad-spectrum antibiotics, and smoking.
Critical Considerations that warrant optimization of oral health in older adult:
- Progressive decline in nutrition resulting from unhealthy food choices, forced by compromised chewing ability.
- Bi-directional association and increased risk of complications from existing medical conditions in presencechronic oral/dental infection.
- Poor oral healthnegative impacts mood and emotional well-being and social-interaction due topersistentoral discomfort, restricted diet andinability to enjoy meals, avoidance from embarrassment due to appearance of mouth.
- Prolonged neglect lead to severe lack of confidence, social isolation and depression that rapidly depreciate the Quality of life of elder adults.
“Increasedlongevitywithoutqualityoflifeisanemptyprize”(WorldHealthOrganization1997)